A mouse study suggests that a common chemotherapy drug may increase the ability of breast cancer cells to metastasize to the lungs. These molecules seem to modify the cells that line the blood vessels in the lungs, allowing cancer cells to more easily enter and latch onto them. This work is published in the International Journal of Molecular Sciences.
Breast cancer is now the most diagnosed in the world. It is also one of the main causes of death among women:685,000 in 2020 for 2.3 million cases diagnosed . Assuming that metastasis is the leading cause of cancer death, it is important to understand the mechanisms behind it.
Previously, researchers had already shown that chemotherapy, which normally helps fight cancer, paradoxically improves metastases indirectly by modifying non-cancerous cells that affect their turn cancer cells. A new study confirms this, pointing out that the increase in the abundance of these cancer cells could be due to an increase in the adhesiveness of the vascular wall.
For this work, the researchers took healthy mice with the common chemotherapy drug cyclophosphamide (CTX). They then waited four days for the subjects to metabolize and excrete the drug. The mice were then injected with breast cancer cells. Finally, the researchers monitored the accumulation of these cells in the lungs.
Compared to a control group that did not receive CTX, the treated mice actually had higher concentrations of cancer cells into the blood vessels of their lungs three hours after the injection.
"The goal of our pretreatment model is to ask the question:Does chemotherapy affect normal cells in such a way that they turn and help cancer cells? The answer is yes “, underlines Tsonwin Hai in a press release, referring to a “warning for the use of chemotherapy “.
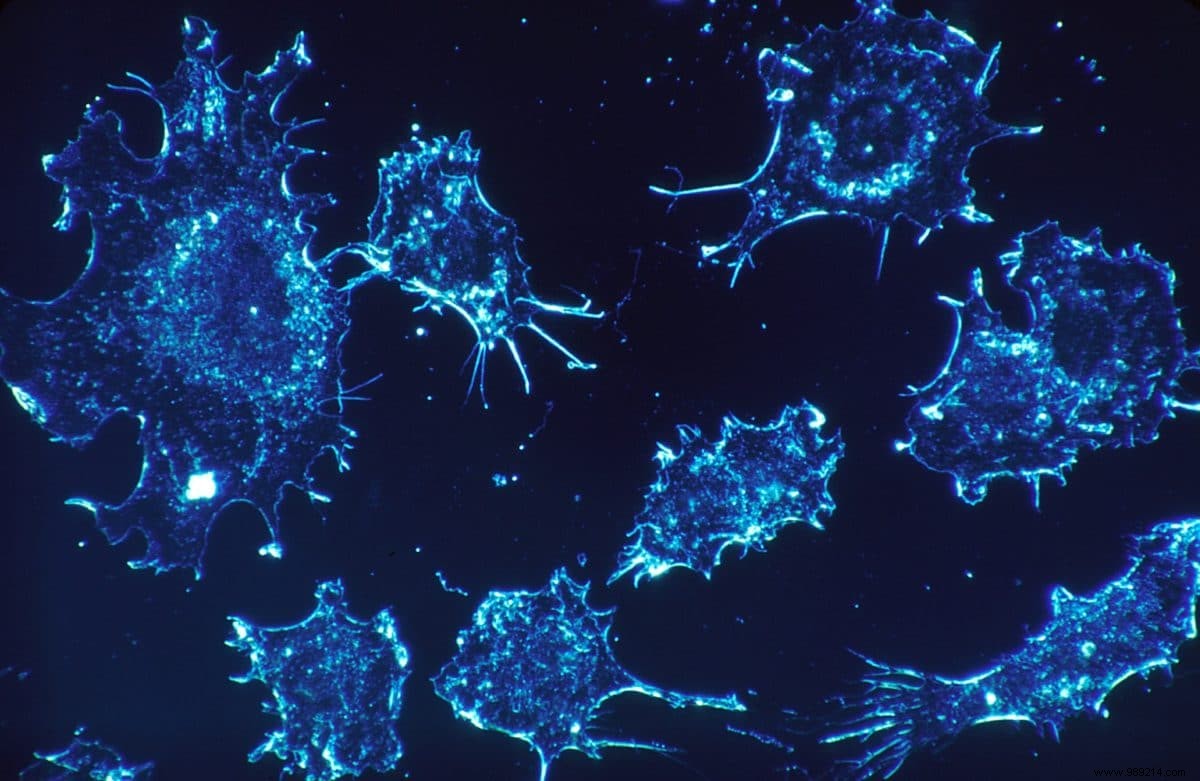
Based on the tests, the drug appears to initially increase the permeability of these blood vessels , altering their underlying basement membrane and allowing cancer cells to "stick" inside the vessels.
“The endothelial cells that line the inner side of the blood vessel are like a brick wall and each brick is tightly glued to the next “, continues the researcher. "What we found when we treated mice with chemotherapy is that the vessel is 'leaking'. So the junction is not so tight anymore and the cancer cells can squeeze through the brick layer “.
According to the study, basement membrane remodeling appears to be regulated by an enzyme called matrix metalloproteinase-2 (MMP-2), levels of which increased after drug treatment. This had the effect of increasing the exposure of two key peptides (RGD and YIGSR) within the basement membrane that both bind to receptors on the surface of cancer cells, ultimately allowing them to latch on.
By adhering to the inner wall, these invading cells then avoid being evacuated by the blood and can therefore settle in the lungs.