Australian researchers believe it is possible that a third wave of Covid-19 could occur. However, this wave would be synonymous with an increased risk of neurological disorders such as Parkinson's disease.
The most common Covid-19 symptom is respiratory distress. However, the disease can also cause neurological disorders , whether encephalitis or anosmia. Remember that coronaviruses are capable of neurotropism, that is to say of infecting nerve cells via different pathways. However, Sars-Cov-2 is no exception to this rule. In their Journal of Parkinson’s Disease publication on September 22, 2020, researchers from the Florey Institute of Neuroscience and Mental Health (Australia) described a rather special case.
It was a 25-year-old female who tested positive for coronavirus. The latter had few respiratory symptoms, had no fever but presented, however, anosmia . The doctors then performed an MRI of the patient's brain and revealed an alteration of the posterior region of the gyrus rectus in the cerebral cortex and of the olfactory bulb. Nevertheless, these alterations resolved after 28 days.
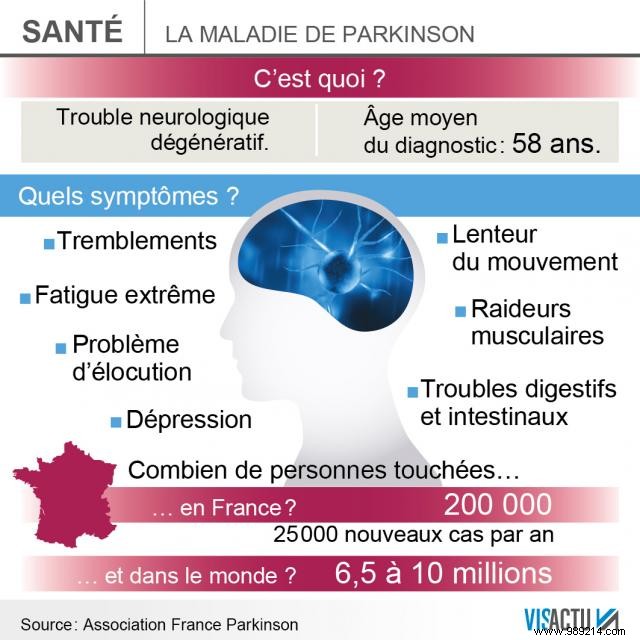
Doctors-researchers formulated a hypothesis, also taking into account other cases. According to them, the pandemic could be prolonged in the form of a third wave . It is not a question here of new infections but of more frequent appearances of neurodegenerative diseases. The doctors mentioned Parkinson's disease. Remember that this disease impacts the dopaminergic neurons of the substantia nigra. This gradually causes tremors and cognitive impairment. If the elements at the origin of the disease are unknown, these are certainly multiple. Specialists believe that inflammation of neurons could be a trigger for Parkinson's disease.
Covid-19 patients have more complement system players, in the area of the brain where neurons die. This sort of innate immune pathway generates reactions that result in the cytolysis of a cell (or a pathogen). According to doctors, this inflammation could be caused by infection with a virus. We also knew that certain viruses cause neurological complications, such as the Zika virus. In the case of Parkinson's disease, certain viruses would increase the risks but nothing has really been proven at this level.
Researchers still mentioned the Spanish flu of 1918. In the years following the pandemic, cases of lethargic encephalitis increased, especially during the winter. Obviously, it was very complicated to study the origin of this problem in the 1920s, but the neurotropic virus hypothesis is relevant. The H1N1 subtype of the virus is therefore a potential suspect. Moreover, the fact is that many Covid-19 patients declared cured still have persistent problems with fatigue, shortness of breath and anosmia. However, you should know that anosmia is present in 90% of people in the early phase of Parkinson’s , a presence up to ten years upstream of the motor symptoms.
In order to follow this potential third wave, doctors propose to create a patient registry Covid-19 having experienced long-term neurological disorders. This will involve giving them blood tests, to observe the possible presence of neurofilaments, and therefore neurodegeneration.